Why did RCPCH decide to develop this work?
Our members are deeply committed to addressing both health inequalities and climate change, which were identified as separate but core priorities in our 2021-2024 strategy.
Following a challenge from Rosamund Kissi-Debrah, who emphasized the need to include health inequalities in conversations about air pollution and climate change, we recognized an opportunity to integrate these two strands of work that had previously been running independently.
We had an existing framework from our earlier policy work on poverty and health inequalities, specifically the #ShiftTheDial on Child Health campaign. Therefore, we decided to extend the campaign into a second year, this time focusing on the connection between health inequalities and climate change.
At the time, few organizations were discussing health inequalities, making it a natural and valuable step for us to contribute to the crowded climate change discourse.
How did you go about it?
The #ShiftTheDial on Climate Change and Health Inequalities campaign was launched in October 2023, aiming to establish thought leadership on both climate change and health inequalities, support our members’ interests and work in these areas, and enhance policymakers’ understanding and motivation to act.
To achieve these objectives, we published a position statement with recommendations for all four UK Governments and educational and advocacy toolkit for paediatricians, and a report summarizing the voices of children and young people (CYP). These materials were approved through various committees, including our Policy and Advocacy Executive and the Executive Committee.
The success of these products can be attributed to thorough planning and collaborative methodologies used.
Theory of Change: Using this model, we defined the problem statement and agreed on broad overarching goals, with success measures at three different timepoints; the end of the programme, following the UK general election and in 2040.
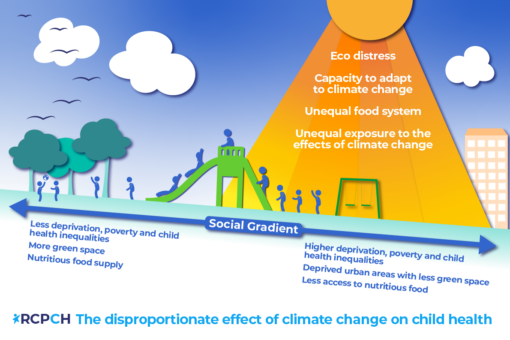
Problem Statement: UK governments have given insufficient consideration to the specific impact that climate change will have on the health inequalities experienced by children and young people.
Overarching Goal: We want UK governments to adequately address the specific impact that climate change will have on health inequalities experienced by CYP.
This approach provided a clear focus for the project and secured buy-in from colleagues across the organization from the outset, facilitating the creation of cross-college working groups.
Cross-College Working Group: This group included representatives from policy teams across all four nations, as well as members from public affairs, media, communications, the brand and design team, the quality improvement team, and the children and young people engagement team.
This collaborative approach ensured that all relevant teams were involved in project planning and development, making it a prioritized workstream across the college from the beginning.
Clinical Working Group: We also established a clinical working group to provide insights into the support our members might need and identify any skills gaps for paediatricians. This group allowed members to share their experiences, which led to the development of an advocacy tool, rather than a quality improvement tool, as had been the case in the previous #ShiftTheDial campaign on poverty.
What challenges did you encounter along the way?
Senior Clinical Leadership: We had a designated Officer for Health Improvement who naturally took on the leadership role for the health inequality aspect of the project. However, we lacked a specific Officer for Climate Change, resulting in a knowledge gap in clinical representation. This gap was addressed through the involvement of the clinical working group.
External Environment: This project was undertaken in a political environment where child health, health inequalities, and climate change were not high priorities. Therefore, our work needed to effectively make the case for the importance of these issues.
What was the outcome and future steps?
We now have a position on climate change and health inequalities and that has become a central theme in all our ongoing work, including our current, more specific focus on air pollution. Finally, we now have an Officer for Climate Change, Dr Helena Clements, who is able to fill the identified gap of clinical leadership on climate change and air pollution projects.
